Texas Medicaid Overview
Historically, most Texas Medicaid services were delivered through the traditional or fee-for-service model. HHSC transitioned to a managed care service delivery model to improve efficiency, care coordination, and early intervention and prevention services. Managed care plans also are able to offer additional services that are not traditionally available in a fee-for-service delivery model.
As a case manager, you must be familiar with the types of Medicaid so you can address your clients' needs effectively. In this section, we'll provide key information about fee-for-service and managed care Medicaid.
Medicaid Eligibility
Medicaid eligibility is financial and categorical. Low income alone does not constitute eligibility for Medicaid. Eligibility factors include:
- Family income
- Age
- Other factors, such as being pregnant, receiving Temporary Assistance for Needy Families (TANF) or having a disability.
Types of Medicaid
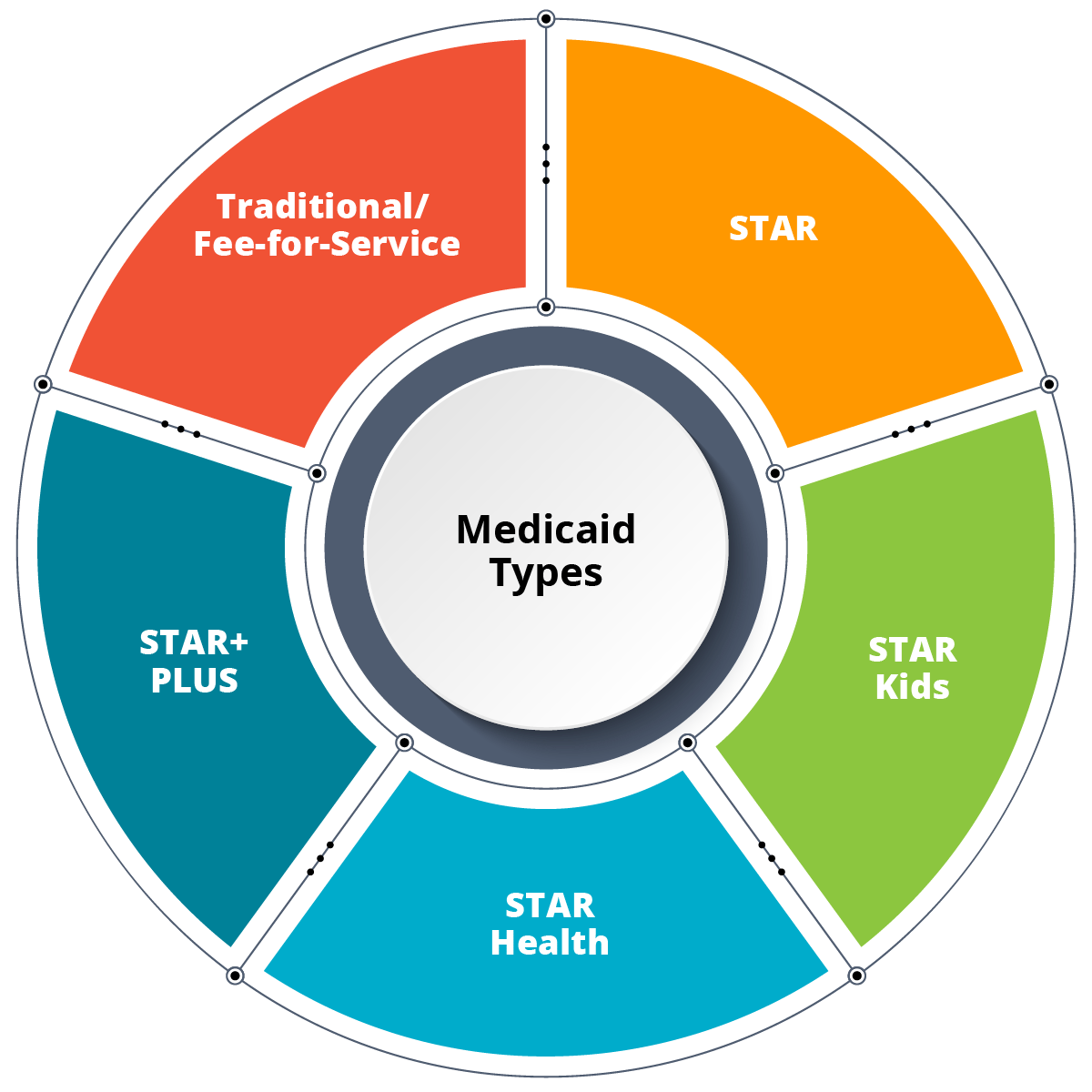
- Traditional or Fee-for-Service
- Managed Care:
- STAR
- STAR Kids
- STAR Health
- STAR+PLUS
Traditional or Fee-for-Service
Clients are placed on Traditional Medicaid when they are initially enrolled in Medicaid. They must pick a managed care organization (MCO) within a designated timeframe or one is picked for them. Most clients are moved to an MCO under STAR managed care.
Managed Care
Clients get their health services through an MCO’s network of doctors, specialists and other providers.
Medicaid Card
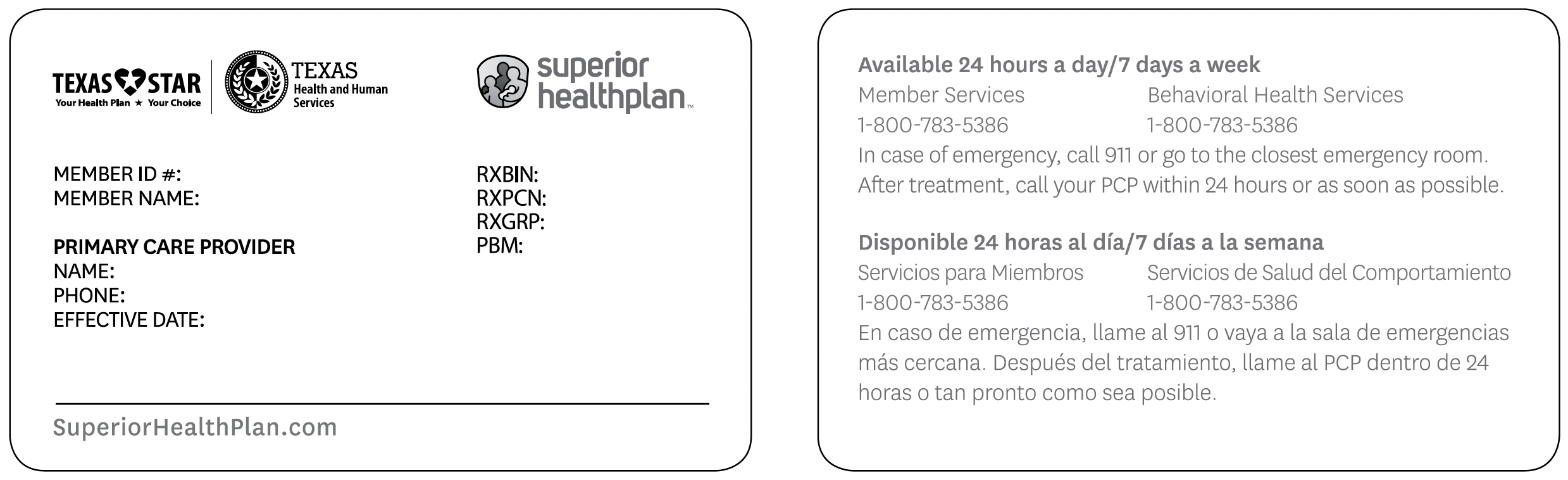
View a sample Medicaid card here.
Clients will also receive a card from their MCO. Here’s a sample:
View the current Medicaid managed care service area map and the Local Health Department and DSHS Regional Public Health Coverage map.
Determining a Client's Medicaid Type
- Know the MCOs in your coverage area.
- List the MCO names when calling the client, parent or guardian at intake.
- Ask the client/parent/guardian if they have a card from an MCO.
- Ask if the client receives SSI.
- Call the Automated Inquiry System 1-800-925-9126:
- Verify Medicaid eligibility
- Indicate Managed Care or Traditional
- State name of the client’s PCP
- Provide the name of Dental MCO
- 15 transactions are allowed per call
- The system is available from 7 a.m to 7 p.m. Monday through Friday
MCO Responsibilities
Each MCO is responsible for addressing the client’s medical needs, including:
- Getting referrals to specialists.
- Helping with transportation to appointments.
- Assisting clients in obtaining durable medical equipment and supplies.
Clients enrolled in an MCO do not need a referral from the MCO or PCP for the following medical needs:
- Eye exams
- OB/GYN services
- Family planning services and birth control
- Mental health services
- Treatment for alcohol and drug issues
- Texas Health Steps preventive medical checkups
- Emergency room services
Note: Each MCO offers extra services called “value-added services.” These may include dental services for pregnant women, as well as health and wellness services. To find out more, visit the STAR Comparison Charts web page.
STAR Kids MCO Responsibilities
STAR Kids provides extra services to include service coordination. Most clients are assigned a service coordinator who will meet with them to address their medical needs. The MCO is responsible for addressing the client’s medical needs to include, but are not limited to:
- Mental health services.
- Occupational, physical and speech therapy.
- Referrals to community services related to medical needs.
CPW Services and Medicaid Managed Care
Clients in STAR, STAR Health, STAR Kids, STAR+PLUS, and the Medicaid-Medicare Plan (MMP) are considered Medicaid managed care members. These clients receive Medicaid-covered services, including CPW services, through their MCO provider network. Only case managers who are enrolled as providers with the MCO can provide CPW services to their members.
Providers will continue to adhere to timelines and provider requirements included in this training and in CPW policy unless otherwise directed by the MCO that the provider is contracted with.
Becoming a provider with an MCO
After completing the Medicaid enrollment process, providers will need to contract and credential with an MCO to deliver services. During the credentialing process:
- You will negotiate rates with the MCO. MCOs are not required to follow the traditional Medicaid fee schedule.
- Make sure to ask the MCO about their prior authorization or prior approval processes.
- The MCO should provide you with a provider manual. This manual contains helpful information about provider services contacts, complaint and appeals, general claims submissions and claims appeals.
Providing CPW services with an MCO
- The MCO will determine whether a member’s case management needs can be addressed by MCO staff, such as their service coordination or disease management staff, or by a CPW provider.
- Providers must submit prior authorization or prior approval requests to the member’s MCO. Make sure to contact the MCO to learn about these processes.
- The MCO will determine whether to allow CPW providers to use the same forms (such as the Family Needs Assessment, Service Plan, Follow-Up, Notes, Referral Form, Case Closure, etc.). Make sure to contact the MCO to learn about these processes.
- The MCO will conduct quality assurance and utilization reviews. Make sure to contact the MCO to learn about these processes.
- Outreach and marketing materials must also comply with Medicaid managed care marketing policies. The MCOs are required to inform the provider of these policies.
Submitting Claims to an MCO
Providers submit claims to and will receive reimbursement from the member’s MCO.
- You will use the same procedure codes and modifiers as in traditional Medicaid.
- You will contact the MCO with any questions about billing for a client in managed care.
When you have a question or complaint
- Providers should contact HHSC CM and DSHS Regional Liaisons to provide CPW policy clarifications and review of outreach and marketing materials for clients enrolled in fee-for-service Medicaid.
- Providers should contact TMHP with questions about billing or prior authorizations for clients enrolled in fee-for-service Medicaid.
- Providers should contact the MCO with questions about billing and prior authorizations for clients in managed care.
- Providers should contact the MCO to file a complaint and exhaust the MCO’s resolution process before filing a complaint with HHSC.
- Providers may file complaints with HHSC if they feel they did not receive full due process from the MCO or if they are not satisfied with the MCO’s determination.
- Providers can mail or email a complaint to HHSC:
Texas Health and Human Services Commission
HHSC-Health Plan Management
PO Box 149030
Mail Code: 0209
Austin, TX 78714-9030
hpm_complaints@hhsc.state.tx.us